

WHO defines sexual health as “a state of physical, emotional, mental and social well-being in relation to sexuality; it is not merely the absence of disease, dysfunction or infirmity. Sexual health requires a positive and respectful approach to sexuality and sexual relationships, as well as the possibility of having pleasurable and safe sexual experiences, free of coercion, discrimination and violence. For sexual health to be attained and maintained, the sexual rights of all persons must be respected, protected and fulfilled.”
Based on this definition, and drawing on the WHO Operational framework for sexual health and its linkages with reproductive health, and from the Guttmacher-Lancet Commission’s report on sexual and reproductive health and rights, HRP’s work on sexual health and well-being spans the continuum from well-being to disease and dysfunction. This includes the prevention and control of sexually transmissible infections, including HIV; prevention and management of cancers of the reproductive system; education, counselling and care related to sexuality, sexual identity and sexual relationships; and sexual function, sexual pleasure, and psychosexual counselling.















In order to develop a short survey instrument to assess sexual health practices, behaviours and health outcomes, WHO has begun a global consultative process. For the resulting draft survey instrument, to be published as a global standard instrument, it is important to first determine that the proposed measures are understandable and relevant worldwide. In 2021, HRP published a multi-country study protocol to assess the interpretability and comparability of the survey instrument.

HRP is the focal point within WHO for preparing evidence-based responses to proposals received from professional societies, academics, and members of the public, relating to all sexual and reproductive health conditions in the International Classification of Diseases and Related Health Problems (ICD). During 2021, responses were prepared on several areas, including abortion outcomes, endometriosis and other gynaecological conditions, intersex-related conditions, and gender incongruence. A detailed evidence review and key informant interviews were undertaken to document the history of the ICD code relating to gender incongruence in childhood. This included the arguments for and against potential modifications or deletions that have been proposed, and whether the existence of a code acts as a barrier or a facilitator to access to care. In anticipation of WHO Member States beginning to use the 11th version of the ICD in 2022, HRP convened several webinars to sensitize users to the changes and support understanding of their correct use.
Reliable and low-cost point of care tests for STIs – which could allow diagnosis and treatment in a single visit – could significantly improve global efforts to monitor, control and prevent sexually transmitted infections. In recognition of this, the second edition of Target Product Profiles (TPPs) for point of care tests to detect four sexually transmitted infections were finalized. Such target product profiles are crucial for the research and development of a target product as they outline its desired “profile” or characteristics aimed at a particular disease or diseases.
Vaccination for Neisseria gonorrhoeae is an important objective for preventing STIs worldwide, as well as for the fight against antimicrobial resistance to existing treatments. WHO preferred product characteristics (PPCs) provide strategic guidance as to WHO’s preferences for new vaccines in priority disease areas. PPCs are intended to encourage innovation and the development of vaccines for use in settings most relevant to the global unmet public health need. In 2021, new PPCs for gonococcal vaccines were published. These describe global public health goals for gonococcal vaccines and preferred parameters pertaining to vaccine indications and target populations, safety and efficacy considerations, and immunization strategies.
New research on STIs is essential to strengthen the evidence base for improved and new interventions and guidelines on several areas. These include: the epidemiology, risk factors, and consequences of STIs; development and evaluation of behavioural, biomedical, clinical, and programmatic STI interventions and strategies; and scaling up existing interventions. In recognition of the need to identify research priorities, HRP supported WHO in its establishment of the WHO Technical Advisory Group on STI Research Priority Setting. Consisting of external experts, the group will contribute to the planning, development, and implementation of the research priority setting exercise.

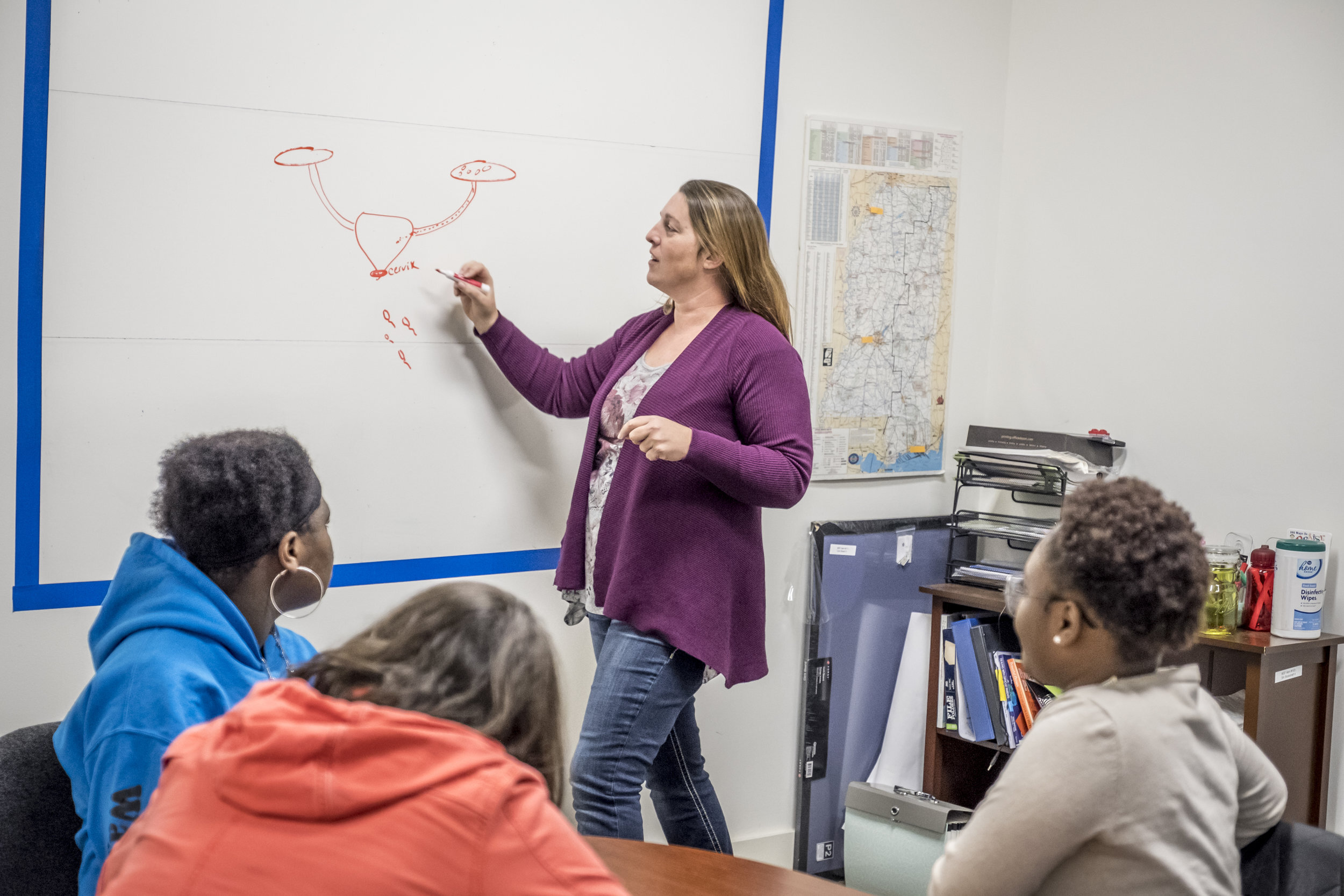
WHO, with HRP’s support, launched a new guideline to help countries make faster progress, more equitably, on the screening and treatment of cervical pre-cancer lesions. New recommendations include a DNA-based test for human papillomavirus (HPV) as the preferred method for cervical screening rather than visual inspection with acetic acid (VIA) or cytology (“Pap smear”), which is currently the most common method globally to detect pre-cancer lesions.
The new guideline includes specific recommendations for women living with HIV in recognition of the fact that they have a six-fold risk of cervical cancer. These include: using an HPV DNA primary screening test, followed by a triage test if results are positive for HPV, to evaluate the risk of cervical cancer and need for treatment; starting screening at an earlier age (25 years of age) than for the general population of women (30 years of age); and retesting after a shorter time interval following a positive test and following treatment.
Access the guideline: https://www.who.int/publications/i/item/9789240030824

In collaboration with the International Community of Women Living with HIV, Trinidad and Tobago, Ukraine, Nepal and three states in India have implemented WHO’s checklist for community engagement to implement the WHO Consolidated guideline on sexual and reproductive health and rights of women living with HIV, as well as the WHO Consolidated guideline on sexual and reproductive health and rights of women living with HIV itself. In addition, young women living with HIV promoted the WHO consolidated guideline during the 16 Days of Activism against Gender-Based Violence, with a suite of infographics which spoke to the specific experiences of violence often faced by women living with HIV – a campaign supported by HRP.